Executive Summary
A wide range of Software as a Service (SaaS) innovations, including artificial intelligence (AI), with demonstrated capabilities to improve patient outcomes, augment population health management, reduce costs, and support the healthcare workforce remain excluded or grossly underutilized in the Medicare program. The Centers for Medicare & Medicaid Services (CMS) operates multiple, siloed payment systems governed by outdated and inflexible regulatory requirements, resulting in inconsistent and often inadequate coverage for software solutions, such as AI tools that make patient-generated health data (PGHD) collected through remote monitoring solutions actionable. Further, the lack of clear, consistent criteria for evaluating and covering new SaaS interventions, combined with price-setting methodologies that do not capture their unique value, discourages investment and slows the integration of potentially transformative technologies into beneficiary care. As a result, Medicare beneficiaries are systematically deprived of timely access to innovations that could improve outcomes and efficiency in care delivery. It is vital that such capabilities are fully leveraged to realize value-based payment (VBP) goals set by Congress long ago.
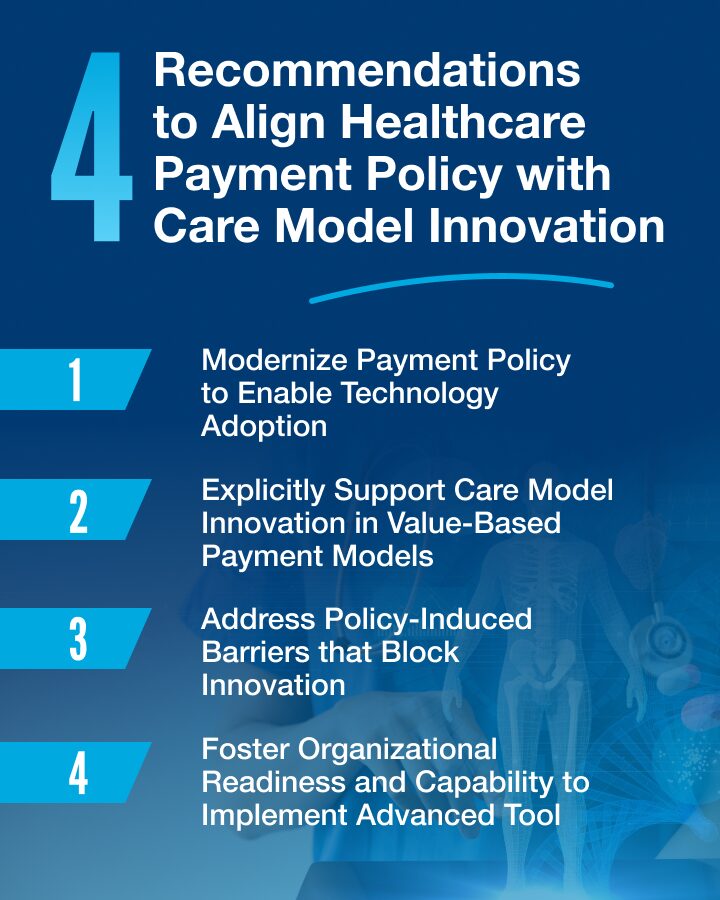
The time for policymaker action to address these challenges is now. To support policymakers in overcoming these barriers, CHI addresses recent payment reform efforts, examines structural obstacles, and offers targeted recommendations to better align payment policies with care model innovation. CHI’s key recommendations include:
1. Modernize Today’s Payment Models to Enable Technology Adoption
2. Support Care Model Innovation in Value-Based Payment Models (VBP)
3. Address Policy-Induced Barriers to Innovation
4. Foster Organizational Readiness and Capability
Ultimately, payment reforms must be deliberately designed to enable and incentivize the adoption of modern SaaS and AI technologies and care model innovation. Removing policy barriers, updating payment systems, and supporting organizational transformation are all essential to achieving the goals of value-based care: improved quality, lower costs, better patient experience, and clinician well-being.